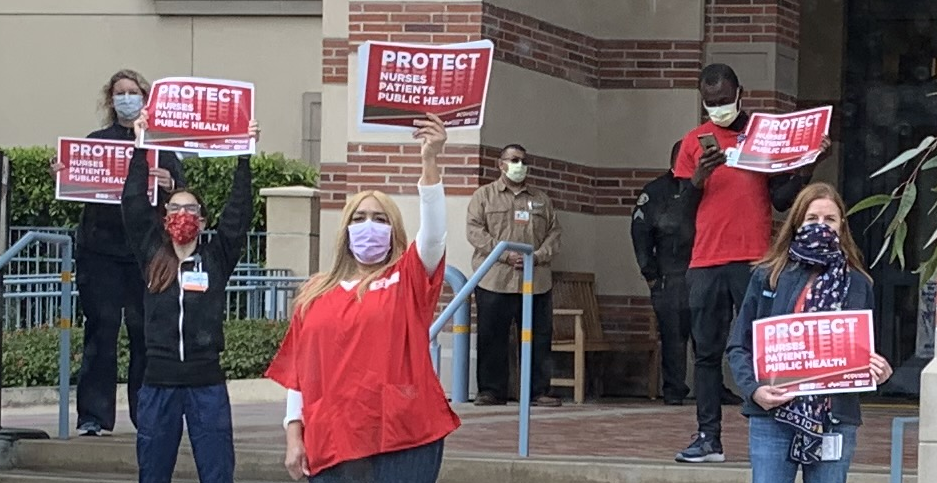
On January 26, nurses across the country held rallies to protest understaffing at a number of major hospitals. The issue, says the National Nurses United/National Nurses Organizing Committee (NNU/NNOC), is chronic and widespread and affects the entirety of the industry. Tempest member Snehal Shingavi spoke to four nurses in Texas who rallied to learn more about the issues and their own experiences as frontline health care workers. This interview has been lightly edited and was originally published in section44.org.
Nurses:
Idali Cooper, RN at Memorial Hospital in El Paso, TX
Juan Anchondo, RN at Las Palmas Medical Center in El Paso, TX
Kellen Gildersleeve, RN in the labor and delivery unit at Ascension Seton Medical Center in Austin, TX
Sylvia Higgins, RN, neonatal nurse at Corpus Christi Medical Center in Corpus Christi, TX
Snehal Shingavi: Let’s start with some introductions. Could you each tell us a little about yourselves?
Idali Cooper: I’m a registered nurse. I’ve been working as an RN for more than 25 years. I’m a mom and a wife. But really, most of my time is spent working. I spend a minimum of 36 hours a week in the hospital. Most of my nursing career has been hospital-based. I’ve worked mainly in pediatrics—I’m currently in the pediatric ICU. I started working as a nurse a long time ago in a combined unit that was pediatric and adult orthopedics.
Juan Anchando: I’ve been working at Las Palmas for 19 years. At the same place and on the same floor. It’s a medical, surgical, and renal floor. We take care of kidney transplant patients, too. I work the night shift. I chose that field because in nursing school they always told us that if you want to get down all the basics and reinforce what you’ve learned, you want to get on to a medical/surgical floor and you can grow into any other field from there. And I took that advice. And the people that were there and that I worked with were really the reason that I stayed. It’s like a family, but even in families, people leave. And there are fewer and fewer people there as years go by. And if other people leave, I may have to leave myself. What keeps me there, too, is that I have seen so much improvement in the quality of care and vision in this hospital—19 years ago, it was such a different animal. Things have gotten so much better since the union came in. There are so many things that used to be done that are no longer kosher now that we have the union.
Kellen Gildersleeve: I have been working in labor and delivery at Ascension Seton Medical Center for nine years (almost to the day!) and I went into nursing because I was interested in midwifery. So I was going to hold out for a labor and delivery position and I was fortunate to get a residency and training in my specialty. I have been at this hospital for my whole career. I am very loyal to the patients I see there and my coworkers. I have been disheartened by the changes that I have seen in the last decade in the profession. There have been so many issues that make it hard to do my job providing care to patients. So, we decided to join a union, National Nurses Organizing Committee/National Nurses United, to demand better conditions for our patients and ourselves. The pandemic was really the straw that broke the camel’s back. A lot of nurses have been dissatisfied with the dismissive response from administration when we bring up important issues.
Sylvia Higgins: I’ve been a nurse for 28 years now. I got into nursing because I like to take care of people. I’ve been primarily in pediatric nursing, and now work in the neonatal intensive care unit (NICU), caring for newborn babies. The union got started in our workplace about 12 years ago. My husband is a union electrician, so we’ve always understood the value of unions. And still organizing in the union for patient safety and care. I was a stay-at-home mom, but when my kids were in school, I knew I had to contribute to the family budget. I was going to go into teaching, but my husband steered me into nursing and it was a better fit.
SS: Describe a day as a nurse at your hospital.
IC: In my unit, we have pediatric ICU patients and step-down patients (not critical, but still need more care than those on the general floor). At the beginning of the day, we give each other reports on our patients, go over the orders, and go over the medications that we have to administer during the shift. Once we are seeing our patients, we take their vitals and do their assessments. We don’t have any ancillary staff (nursing assistants and a unit clerk) in our unit. When I first started working on a general pedes floor, we always had ancillary staff. At another hospital where I worked, we had ancillary staff. But here we don’t and I don’t understand why – they are just trying to save money.
JA: I put up my stuff and go get my assignment and patient roster. I talk to the nurses who had the patients that I am assigned to—that can take between 20 minutes and an hour and a half. I’m getting information on my patients, looking at labs, figuring out what’s pending (like a doctor has ordered a study), and figuring out what scans still need to be done. And sometimes the equipment is down, or the computers go down, and we have to work around that. We have to prepare all of the patients’ medications.
We do assessments on the patients, head to toe. Occasionally we find that there is something else going on other than what they came in with. Clots that move throughout the body, or shortness of breath which might indicate that a clot has moved to their lungs. We get patients who come in with abdominal pain, and they might go in for surgery in the morning, and we take care of them until their good enough to go. Pre- and post-surgical patients, as well. So at night, we dispense meds and make sure that patients are sleeping okay.
We have patient care techs who help you, but sometimes they are overextended. You need two or three people, sometimes, because we have patients that need help to walk or are bed bound. You need multiple people to help with patients who are incontinent or don’t have catheters. We pay close attention to acuity—let’s say a patient is on IV fluids and has a feeding tube and they have sores on their body—you are there and you have to mix the meds, make sure that the IVs are good and functional, there can be multiple problems with a single patient and you stay with that patient to deal with all of those issues. And you can have another patient who just has a single issue. You can have six patients one day (what we call “walkie-talkies”—ambulatory and talking) and it’s not so bad, but other days you can have fewer patients and it’s really bad because all kinds of things can happen. If you have all of these problems in a single patient, you have a higher acuity level.
We still have support staff, but there is definitely a slowdown in hiring. Certified Nurse Assistants (CNAs) are definitely preferred to Patient Care Technicians (PCTs), but as the CNAs leave, they are replaced by PCTs. A PCT will just take the vitals, but a CNA will intervene immediately when they see a problem in taking down information because the CNA knows what to look for. We rely on them because they are an extension of us, and they keep us informed of changes in our patients.
What I have found is that PCTs don’t know this, because they haven’t gone through the same training that CNAs have. It’s a little disturbing that we have to train our PCTs on how to do their job, because they simply aren’t equipped to. They don’t really know what they are looking for when they read the data. They don’t get the gravity of not letting us know in a timely fashion because of how fast things can escalate.
KG: For the past three years, I’ve been in the maternal transport position.
Essentially, if there are really sick pregnant people in surrounding Austin hospitals that need to be in our unit (which is a high-risk obstetrics unit), then I can go in an ambulance or helicopter to accompany them and make sure that there is a nurse with them. It can be a scary experience for patients, so it is important to be there, and to have someone with obstetrics expertise. And when I started, I was always able to accompany those patients. But staffing has gotten bad enough that there are multiple shifts a month where I have patients to take care of at my home hospital and so I’m not available to transport patients. Short-staffing can cause delays to excellent care.
It’s frustrating because we’ve established this amazing Maternal Transport program that we were very proud of, but the lack of staffing means that we can’t actually achieve our goals. Staffing is so poor that there isn’t always a nurse to accompany patients on their journey. On top of that, we work 12.5-hour shifts. We’re on our feet most of the day. There is no lunch break on many days, so we don’t get to hydrate or eat regularly. And these arduous working conditions make for dangerous patient conditions.
SH: In my unit, a neonatal ICU, our nurse-to-patient ratios are pretty small. Typically, in the NICU, I have three babies that are level two, which is a step below a critical baby, but we also have level three babies who are critically ill and have only one assigned nurse for each baby. These are babies on ventilators. In our unit, our ratios are enforced pretty well. I’m more concerned with the units like medical/surgical or ICU where the staffing turnover is greater and they are chronically understaffed. I care for babies who need to learn how to eat—bottle feed. People don’t realize that babies are not ready for bottle feeding. I feed them every three hours and take care of their needs and medicines. Every so often we get a baby that needs an IV for antibiotics. I work 12-hour shifts. We are constantly monitoring our patients. Preemies can suffer from necrotizing colitis: where their intestines are not absorbing nutrition effectively and then they require critical care. We can also have babies whose mothers are on opiates, and the babies have opiates in their system, and we have to help them withdraw from these drugs.
SS: Tell me why you joined the union.
IC: I think that because I worked in union hospitals, and I transferred to a new hospital when they opened a children’s hospital and closed our floor. They told us that we couldn’t refuse patients, even if we didn’t have the personnel to deal with them. The union gives us a voice to be heard. At a non-union hospital whatever administration says goes.
JA: The union started in our facility, I believe it was around 2010. I saw the merits of a union in my family growing up. My dad was a shop steward at a union at ASARCO, and they were a strong union. I remember that as a kid, I wouldn’t see my dad all that much. He was exhausted all the time—part of the maintenance staff. And when he was out on strike and he would take me to a picket line and we would march. And for me it was a good time, I got to spend time with my dad, but I also learned why he was doing it, for a better life and better working conditions.
It was about health and safety for them, and when ASARCO didn’t want to change, it was the union that helped to push them. People were endangering their lives working there. People had to get tested regularly to see how much arsenic and lead there was in their blood. They were poisoning their bodies to provide for their families. And if they had to go on strike, they went on strike. The union had a strike fund and paid a stipend if you picketed. But we would go collect cans and cardboard boxes and sell those for money—it felt like fun and playing to me. I don’t remember us ever going hungry. I’m sure it was tough on my dad, but to me, it was everything to have time with my dad.
I knew the merits of the union before the NNU came. So when they started organizing, I told my coworkers about my experiences. If you go to management by yourself, they can ignore you. But collectively we had power.
KG: I have had my eye on unions for many years as being a possible solution to some of the systemic issues that we have seen in my industry and at my hospital in particular. Unions had achieved so much in California—breaks, staffing ratios, appropriate wages. People here were afraid to talk about unions and would tell me not to bring it up again when I would broach the subject. I would get shut down a lot. When those same nurses who had previously expressed fear about unions started discussing them more positively, I knew that something had shifted. Nurses in El Paso and Corpus had won unions.
A lot of nurses began to feel that something could change, and we did make a change. Equipment availability has been a big issue, especially with the supply chain issues: PPE, IV pumps, blood collection tubes, and medication shortages. All of these affect our workflow and increase the risk of error. We have been concerned by the failure of administration to anticipate and deal with these issues. They aren’t getting us what we need or preparing for our future needs. It seems like a conflict of interest with them keeping the budget so tight while claiming to provide the highest quality of care.
SH: I joined the union because I believe that workers should have a voice and be united in working together to make sure we are treated fairly. We should be listened to by administrators when it comes to staffing, having working equipment, getting fair wages, and that our rights are protected.
SS: What were the issues that made you come out to the rally on Thursday?
IC: My union, NNU/NNOC, we were doing a national day of action to advocate for better and safer staffing. I feel like staffing never recovered from the pandemic. We lost a lot of nurses. We had a mass exodus of nurses from the hospital, taking traveling jobs, and the hospital never recuperated those losses. It’s probably a combination of a lot of things. After the pandemic, the nursing profession changed, nurses became more valuable, nurses went to jobs offering more money, and the hospitals have been unwilling to increase pay. There are certain hospitals that are offering more money, and other hospitals are not keeping pace. It’s also a matter of safety.
Because we are short-staffed, nurses have to take on more patients. Most of us feel like we’re being stretched. We are working with a skeleton crew and nurses are getting tired and burnt out. Morale is down. During the pandemic, since the administration was asking us to work in unsafe environments—because they weren’t offering the PPE that was necessary—a lot of nurses retired. A lot of nurses wanted to continue working, but once COVID-19 hit, a lot of nurses retired because they weren’t going to put their lives on the line. I hear nurses saying that due to their mental health, they are cutting down their hours—for their emotional, mental, and physical health.
JA: The national day of action was about hospitals investing in safe staffing—it was an action for the whole country and the whole industry. Profit-driven health care has created this problem. There is no nursing shortage—nurses have left for better-paying jobs as traveling nurses or as contract nurses. Nurses will leave and then come back as contract nurses. Some people will leave hospitals because of the stress. We call it “morale distress.” The conditions in profit-driven hospitals are terrible.
We have a staffing grid. If you have so many patients, you get so many nurses. Let’s say you get six nurses. But you show up, and there will only be five nurses, because management will say they have to make up hours or that they are over budget and they won’t call everyone in. And then you have to do what you have to do to deal with being understaffed. We plow through and take care of patients as best as we can, but you will be mentally exhausted from all of the work. Or let’s say you have eight nurses scheduled, and seven come in, but then they float one of your nurses to another floor, and that happens a lot. Understaffing is a chronic problem.
The nurses’ union has done surveys, and close to 3000 nurses responded, to find out about staffing. The majority of people responded that staffing had gotten worse or much worse recently. And the band-aid that the hospitals produce—contract nurses and traveling nurses—aren’t sustainable. There are a lot of nurses in El Paso. People will leave and go to other hospitals, like William Beaumont Hospital or UMC (University Medical Center), because they are tired of working in short-staffed conditions or because they can get better pay. Management here doesn’t seem to care, and nurses feel appreciated at other places. They can get retention bonuses and other perks.
KG: I was inviting people out to the vigil in Austin, part of a Nationwide Day of Action for nurses. We were mourning Ascension’s lack of commitment to patient safety. Our concerns are rarely addressed. We are told that our issues are not important. We wanted to show the community, and Ascension, how important patient care is to us. The vigil was specifically a response to the moral injury that we have undergone as nurses, consistently being asked to do more with less and watching our patients suffer as a result. For most shifts, we can only do the bare minimum—and that is not what we got into the profession for. In the system that we are working under, it can feel like you are doing more harm than good. We wanted to bear witness to the failure of this Catholic Health Ministry and its mission to serve the community. People want their loved ones to be taken care of with the appropriate amount of care and attention that they deserve.
For several months this summer, we were not able to electively induce patients who wanted to have their babies. If someone was ready to deliver their baby at 39 weeks, previously we were able to fit them in them right away. Patients expected to have this option available to them. However, we were only able to accommodate medically indicated deliveries for higher-risk pregnancies. And pregnant patients who were miserable, because the last trimester is physically and emotionally taxing, could not be helped. That’s just one example of how shortages in staffing have directly affected our patients.
SH: Inadequate staffing levels, for sure. A lot of nurses have left because they didn’t feel valued. The pandemic really shook up our industry. We wanted to speak out and bring attention to our working conditions. Nurses have left and the hospital hasn’t replaced them. Nurses work long hours, they don’t have time to take lunch breaks due to short staffing. They don’t get assistants to help them with their patients. This is why union members speak out about staffing. Nonunion nurses can’t speak out. It’s a crisis because nurses aren’t valued, recruited, or retained—we are overworked and underpaid.
SS: So why do you stay at your hospital?
IC: Nursing jobs are rewarding because our jobs make a difference in people’s lives. We like to help people. That’s why I got into this work.
JA: I like the people that I work with. I like my days off, but I want to see my friends again. I go into a chaotic situation sometimes, but if you have your friends, you can get through everything. I love what I do. I like to see patients get better. They came in sick and leave better. You see them around time, and you feel like you participated in their lives and their well-being. I know the conditions of that hospital, and how it was before, and I am helping that place get better. We have to drag management kicking and screaming to make things better, but we do that with the union. All management is looking at is dollar signs, and all we are looking at is better patient outcomes. That is what we are there for. Our passion is helping our community and our patients.
KG: I have personal reasons for staying, but beyond that, the unit that I work on was an amazing unit to work on when I first started. And I think that we can get back there if we convince administration to make some changes. I feel hopeful because I was committed to unionizing, and I wanted to see that through. I feel more committed than ever to making a difference. And unionizing has given me hope in nursing again, despite the fact that many other nurses have become understandably cynical.
Sylvia Higgins: I love my job. I feel fortunate that I am still able to do my job. The best thing about it is when I am able to discharge a baby to go home and the mother is able to feed and take care of it. I used to work pediatric oncology and that was hard. At this job, babies go home to be with their mothers.
SS: What is it that you want your hospital to do?
IC: We want Tenet to provide us with safer staffing, more nurses, safer working environment. I just want us to go back to the previous number that we had in our hospital—we’ve lost at least 30 percent of our nursing personnel in our hospital. That’s a common experience for nurses in hospitals everywhere.
JA: Our union is made up of bedside registered nurses. So we know what is needed to help hospitals retain their nurses. And we want them to hear us out. Because we know what patients need. Management is not doing enough and they think that they know better. We call out management when they try to justify their actions. They cannot retain their nurses doing what they are doing, and we know what it will take to keep nurses around.
KG: We want our hospital to help us retain hospital staff with better wages and better ratios, so that people aren’t going home with moral injuries. We want a process of nurse-elected administration so that changes in practices are not unilateral and we have a say in how those changes are made.
SH: I want the hospital to support the nursing staff, to acknowledge the nurses that stayed through the pandemic and didn’t go somewhere else. I want the hospital to staff appropriately and do more to recruit and retain nurses. HCA is no longer offering incentives for extra service. Meanwhile, HCA’s profits have gone through the roof.
In 2019, HCA was planning on laying off a lot of nurses, but the pandemic hit and they needed nurses. They threatened to take away our contracted pay increases, but they couldn’t do that because we have a union. They threatened to take away the matching funds to our 401k, and we fought them and won. They do everything that they can to increase their own profits at the expense of the nurses.
SS: What do you want people to understand about your protests and your reasons for rallying?
IC: Taking care of people and their loved ones is important to us, and we want to do that in a safe and high-quality manner. And even though the hospital says they have safe staffing, they are not being truthful. All we want is to be able to take care of our patients and deliver high-quality care. We also want the public, and they have always supported us, what we want is to support them by getting better patient-to-nurse ratios. California has a law that dictates how many patients a nurse can have. We would like the community to support us by pressuring legislators to pass a similar law here. During the pandemic, President Biden actually helped us pass an OHSA standard to ensure that nurses had sufficient PPE, and that we didn’t have to reuse PPE, but this was temporary. We want the public to convince OHSA and the government that these standards become permanent. This wouldn’t only protect nurses. It would also protect every health care employee.
JA: We come out to rally because the hospitals get defensive and try to cover up what’s really going on. I think people need to understand why nurses care.
KG: I think that the vigil was important to me personally because it was our opportunity to show the community that we are fighting for them in every way that we can. We are going to need community support going forward to make sure that Ascension and hospitals across the city are held accountable. Patients who have the ability to do so need to speak up and help us address these problems.
SH: I want people to know that nurses are just asking for adequate support from the hospital. That our staffing ratios are met, that we have assistants that we need, and that we can even take our lunch breaks when we are supposed to. This is why we have nurses who are exhausted and feel moral distress because they can’t give patients the care they deserve.
I joined the union because I believe that workers should have a voice and be united in working together to make sure we are treated fairly. We should be listened to by administrators when it comes to staffing, having working equipment, getting fair wages, and that our rights are protected.
SS: Tell me about your coworkers.
IC: My friend also works in an ICU in the hospital. Also having a hard time. They have three patients all the time; the maximum should be two to one. When they have three patients, they can’t adequately take care of them. The patients will regularly have falls because nurses can’t always keep an eye on them. Their drips aren’t weaned properly because we can’t be there to do it. So, you have a greater risk of IV infiltrations. And you have more failures to rescue: if you don’t have the time to get to your patient, the risk of death becomes a lot higher.
My friend had to move to a part-time position because he couldn’t deal with the stress of the higher patient load. This is just asking for our patients to be safe. Usually, after we see our patients, we have to do a lot of documentation for the hospital, and when we have more patients than we should, we don’t have the time to document everything until the end of the shift. Administration gets upset because we can’t do it in a timely manner, but we don’t have the staff to do that. And that means we have to stay late, then we sleep late, and then we’re tired the next day. There is a lot of research out there saying how unsafe it is when you don’t have adequate nursing staffing. The greater the number of patients that we have the greater the risk of medical and administrative errors.
KG: I work with really amazing nurses—passionate, intelligent people. Before I was in the union, I only talked to nurses on my floor, but once I started organizing, I started developing friendships across the hospital. My coworkers are the reason that I am able to come back to work every day despite miserable conditions, and I am grateful for them.
SH: The core of us who have stayed have a love for our work, and love working with babies. There is always teamwork in my unit. Babies can come in twos and threes sometimes, and then you need all hands on deck. We have even had to call in nurses who are off and they come in because they love to help. You can always count on the coworkers in my unit—they’re amazing.
SS: Any final thoughts?
IC: When we do commit errors, the hospital wants to write us up and reprimand us, but at the end of the day, they are the ones that should be reprimanded for not providing the adequate staffing that we need.
JA: Besides them hearing us about how to retain nurses, the nurses’ union has also sponsored legislation at the federal level. There’s a bill that would mandate a minimum nurse-to-patient ratio. They have that in California—the CNA (California Nurses Association) helped to pass that. For us, it’s the golden rule, because there are penalties for hospitals that don’t meet those minimums. During the pandemic, of course, there were exceptions, but even then we found that hospitals were keeping staffing levels low to keep a profit. The turnover rate of nurses in Texas is triple that of California, and it’s primarily because of the staffing ratios. The research shows that when the nurse-to-patient ratio is low, you have better outcomes, improved patient care, and lower mortality rates.
KG: Typically, when a nurse enters the field, you go in thinking you can help people in difficult times, and then you are hit with the reality of for-profit care, the unethical solution that we have landed upon, and it is awful. What is happening with health care in this country is a disaster and we have to organize as nurses collectively to advocate for our patients. This problem is too big to tackle alone. It has to be done collectively.
SH: We need more nurses and better facilities. We have an ER that is chronically overcrowded, with patients in the hallways. I’ve been there 15 years, and the size of that ER hasn’t changed. And HCA has the money. If there were better staffing, people wouldn’t have to wait for hours. I would love to see HCA use its profits to improve the environment in the hospital—make the building and equipment better. Sometimes housekeeping is lacking because they are short-staffed, and sinks aren’t cleaned or trash isn’t taken out.
Featured Image credit: Nevena Pilipović-Wengler.